If you are confused about the difference between colon polyps and colon cancer, that’s understandable. With National Colorectal Cancer Awareness Month right around the corner in March, it’s the perfect time to clarify any uncertainties surrounding our colon health.
The most important thing you should know is that having colon polyps does not mean you have colon cancer. In fact, most colon polyps don’t progress to become cancerous. However, because nearly all colon cancers start as polyps, it is important to understand what they are and what should be done in the event they are found.
What are polyps?
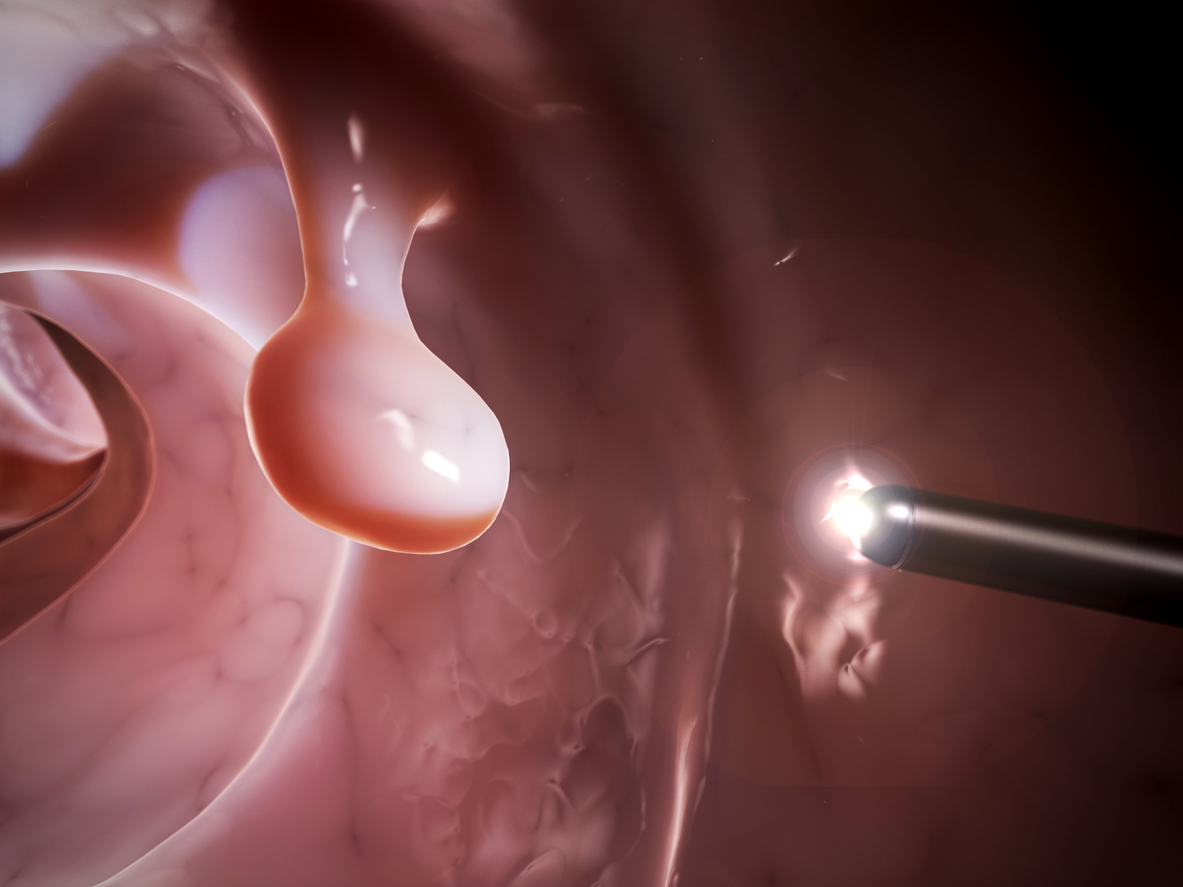
Colon polyps are small growths that form on the inner lining of the large intestine or rectum. They can range from a few millimeters to several centimeters in size and can be flat or raised. These growths are typically noncancerous, but they have the potential to develop into cancer over time – if left untreated.
What causes colon polyps?
Your environment and genetics play a role in whether you develop colon polyps. The following factors can increase your risk:
- High red meat consumption—Eating lots of red meat, particularly processed meats, increases the risk of colon polyps and cancer. Compounds in red meat can harm colon cells during digestion.
- High-fat diet—Diets rich in saturated and trans fats raise colon cancer risk. Fatty foods can negatively affect colon cells, promoting polyp formation.
- Low-fiber diet—Fiber aids digestion and colon health. Diets lacking fiber may prolong exposure to carcinogens and toxins in the colon.
- Smoking—Smoking chemicals can harm colon cells over time, boosting polyp and cancer risk. Quitting smoking lowers this risk.
- Obesity—Being overweight ups the chance of colon polyps. Fat cells may release hormones that spur polyp growth, while obesity-related inflammation could also contribute.
- Alcohol intake—Heavy, regular alcohol consumption heightens colon polyp risk. Alcohol may irritate and facilitate carcinogen penetration into cells.
- Genetics—Inherited genetic mutations can significantly increase susceptibility to colon polyps and cancer. Be aware of your family history.
Symptoms of colon polyps
Most colon polyps do not produce symptoms. This is why screening is vital to detect them. Occasionally, individuals may notice red or black blood in the stool when polyps bleed. This may be intermittent. It is always important to notify your doctor immediately if you see blood in your stool.
” Many people worry about polyps, but the most important thing to know about colorectal health is that screenings and early detection are key to preventing colorectal cancer. My #1 recommendation—get your colonoscopy. “
Albert Youn, MD
Welia Health General Surgeon
Colonoscopies save lives
While many people are anxious about colonoscopies, they are essential to routine preventive care for adults. The American Cancer Society recommends all people with an average risk of colon cancer get their first colonoscopy at age 45 and continue them every 10 years through at least age 75 if they’re in good health and have a life expectancy of 10 years or more.
If you’re 76 to 85, your provider can recommend whether or not you should continue screenings.
People over 85 should no longer get colorectal cancer screening. However, you may wish to discuss this with your family medicine provider.
If you are at higher risk of colon cancer, you may need to begin colonoscopies sooner and potentially have them more frequently; for example, if you have:
- A personal history of certain types of colon polyps, colon cancer or inflammatory bowel disease like Crohn’s disease or ulcerative colitis.
- A personal history of radiation therapy to the pelvic or abdominal area for previous cancer treatment.
- A family history of colon cancer.
- A diagnosed or suspected hereditary colorectal cancer syndrome, such as Lynch syndrome or familial adenomatous polyposis.
While colonoscopies are considered the gold standard in colorectal screening by most doctors, less invasive screening options are available. Note that if you are at higher risk, the recommendation would still be a colonoscopy over less invasive testing. See Colonoscopy and Cologuard: The pros and cons, from Welia Health Connections for more details.
Treating colon polyps
The colonoscope used during a colorectal screening uses a small flexible tube with a light and a camera is inserted into your rectum to look at your colon. This tube is also equipped is a snare-like device that can grab and snip off polyps if they are relatively small.
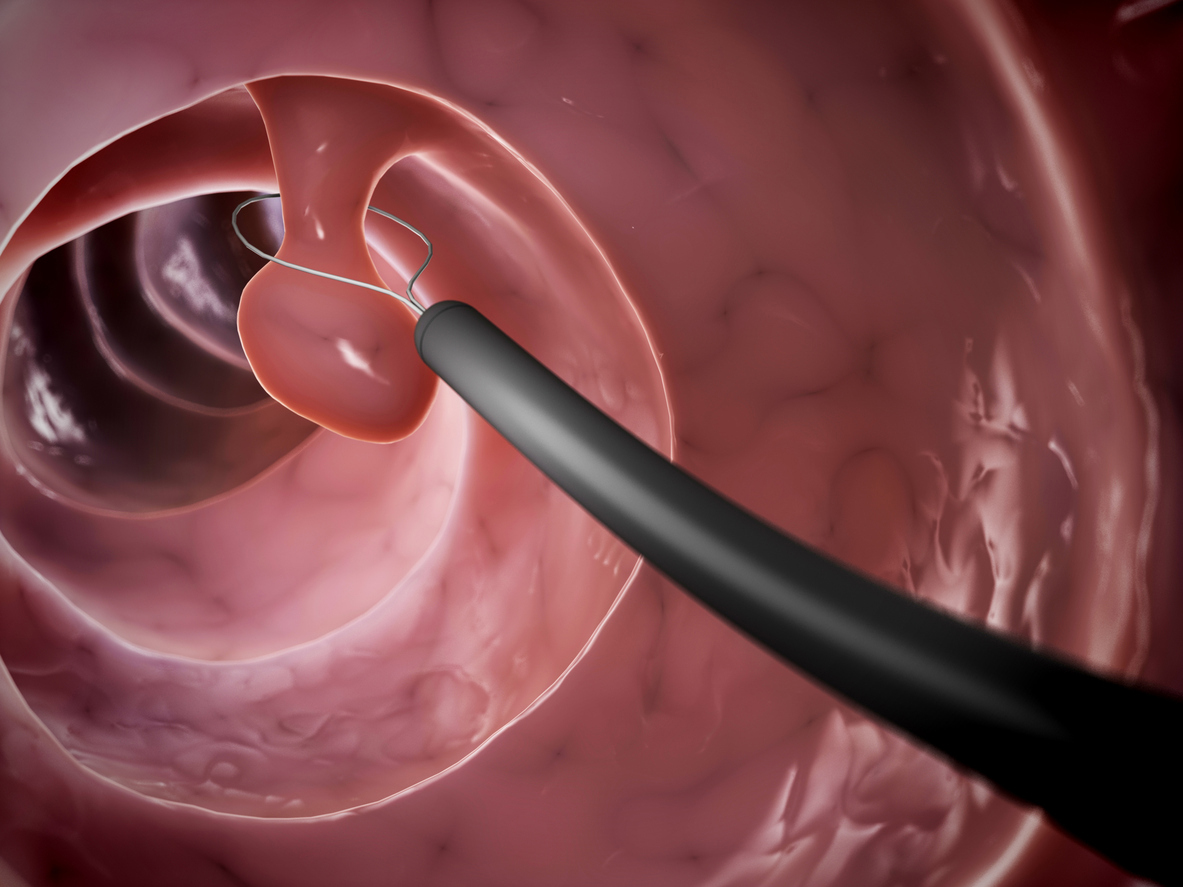
- If the colonoscopy finds one or two small polyps (5 mm in diameter or smaller), you are considered at relatively low risk. Most people will not have to return for a follow-up colonoscopy for at least five years, and possibly longer.
- If the polyps are larger (10 mm or larger), more numerous, or abnormal in appearance under a microscope, you may have to return in three years or sooner.
- If the exam finds no polyps, you can usually wait 10 years for the next screening if you are at average risk for colon cancer.
Regular screenings can even prevent the development of cancer. It may take up to 10 to 15 years for a polyp to evolve into cancer. Through screening, your provider can identify and eliminate polyps before they progress to cancer.
What is colon cancer?
Colon cancer ranks as the second leading cause of cancer-related deaths in the United States and worldwide. Originating in the large intestine (colon) or rectum, it typically begins as a small, benign polyp that very gradually transforms into cancer.
Early screening can often detect colorectal cancer when it is still localized and more manageable.
Symptoms of colon cancer
In many cases, there are no obvious signs of early-stage colon cancer. If polyps are undetected and cancer develops, symptoms that can develop over time include::
- Rectal bleeding or blood in stool—A common sign of larger polyps is seeing bright red blood during a bowel movement. It is critical to discuss any gastrointestinal issues with your provider right away.
- Changes in bowel habits—Polyps that partly block the colon can cause constipation, diarrhea, or changes like narrowed stool. Sudden unexplained changes require medical attention.
- Unexplained iron deficiency anemia—Long-term blood loss from a large polyp can lead to low iron levels and anemia, requiring tests to find the source.
- Abdominal pain—Large polyps may cause cramps, pain, or tenderness in the lower abdomen, typically easing after removal.
- Weakness and fatigue—Anemia from blood loss can cause abnormal tiredness, weakness, or breathlessness, needing tests to check for colon polyps as the cause.
- Unexplained weight loss—Significant unintentional weight loss could signal a large, advanced polyp or colorectal cancer, prompting a doctor’s visit for diagnosis.
Colon cancer treatment
If diagnosed with colon cancer, treatment options may involve surgical procedures to remove tumors or affected parts of the colon or rectum, chemotherapy to eradicate cancerous cells, radiation therapy to target tumors, targeted therapy medications, immunotherapy, participation in clinical trials, or palliative care to alleviate symptoms and enhance the quality of life.
For more information on colon cancer, visit the American Cancer Association website.
Get screened to prevent colon cancer.
It’s important to remember that colorectal cancer is one of the most preventable forms of cancer—if you are screened for hidden warning signs while you are still healthy. Call Welia Health at 320.679.1313 to talk to your provider about scheduling your colorectal screening today.






