Empowering our community with knowledge
Opioid overdoses are a serious public health crisis worldwide, in the US, Minnesota and our communities, too. According to the National Institutes of Health, the statistics are brutal – more than 9 million Americans ages 12 and older misused opioids in the past year, and more than 5.5 million live with opioid use disorder.
Overdoses from opioids can be fatal. The Centers for Disease Control and Prevention (CDC) estimates that over 108,000 people died from overdose in 2022. Most of these deaths involved opioids. However, with the right tools and knowledge, we can save lives. An opioid overdose can happen at any moment, leaving its victim hovering between life and death, but with Naloxone (more often referred to by the brand name of Narcan®), the medical community finally has a tool to counteract opioid’s deadly impact. Working wonders in the brain, this therapy reverses the opioids’ hold, enabling people to breathe and increase the chance of survival.
Naloxone education is a priority of Welia Health’s community outreach efforts, and for good reason—it has the potential to be a lifesaver. The three minutes you spend reading this post could just save a life. We’ll take you through the anatomy, functionality, and availability of Naloxone so you’re prepared in an emergency.
What is Naloxone?
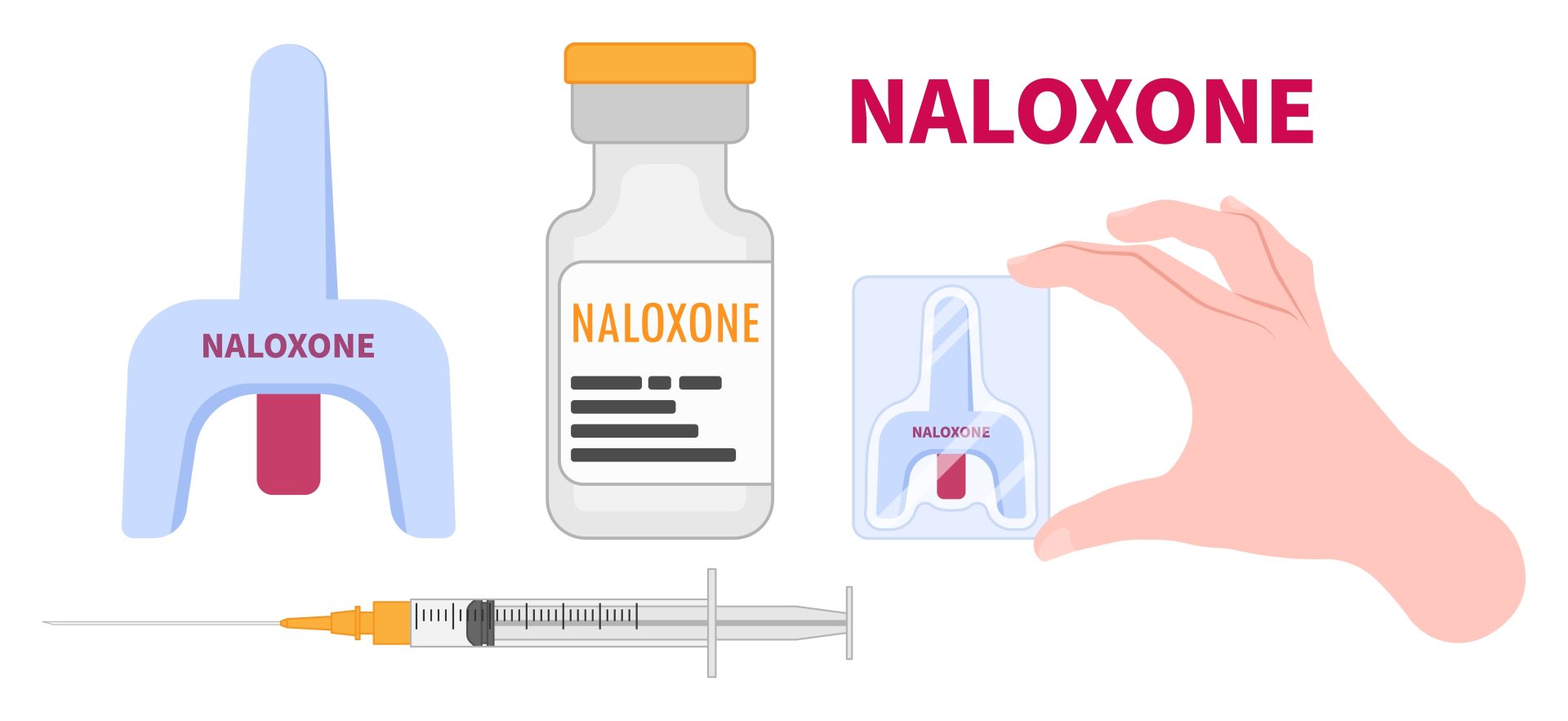
With opioid overdoses on the rise, Naloxone offers a glimmer of hope – a swift, reliable way to counteract the drug’s lethal grasp and restore life-saving rhythms. This opioid-blocker function effectively rejiggers brain chemistry to reboot regular breathing. Naloxone is available in two forms:
- Injection: This form of Naloxone can be administered by healthcare providers and is also available for use by anyone. It is distributed through the Naloxone Access Point. If individuals lack insurance or cannot afford the nasal formulation, they can receive a free kit containing the injectable form.
- Nasal spray: This form of Naloxone is user-friendly and can be administered by anyone, including those without medical training. It is preferred due to its ease of use.
Signs of an opioid overdose
It is important to be aware of the signs of an opioid overdose so that you can take action quickly. Here are some of the most common signs:
- Shallow or slow breathing, or breathing that has stopped altogether
- Blue-tinged lips or fingernails
- Pale, clammy skin
- Small pupils
- Confusion or drowsiness
- Seizures
- Vomiting (may or may not be present)
The National Library of Medicine offers an overview of opioid overdose and Naloxone administration.
How to administer Naloxone
If you suspect that someone is experiencing an opioid overdose, call 911 immediately. While you wait for help to arrive, you can administer Naloxone if it is available. Here are the steps on how to administer Naloxone nasal spray:
- Remove the spray from its packaging.
- Position the person on their back.
- Place the tip of the nasal sprayer into one nostril, tilt the head back, and firmly push the plunger.
- If trained and comfortable, perform CPR while waiting for a response.
- If there is no response after 2-3 minutes, repeat step 3 in the other nostril.
- Stay with the person in need until the EMTs take over.
Read more about opioid overdose.
Important facts about Naloxone
Here are some additional things to keep in mind about Naloxone:
- Naloxone is safe to use, even if the person does not have an opioid overdose.
- Naloxone will only reverse the effects of opioids. It will not work for overdoses of other drugs.
- The effects of Naloxone wear off after 30 to 90 minutes. Depending on the situation, more doses of Naloxone may be necessary.
Where to get Naloxone
Naloxone is available without a prescription at many pharmacies. Welia Health is proud to be an accredited Naloxone Access Point. This means that we can provide free Naloxone kits to anyone in the community.
Not only do Naloxone kits contain the medication itself, but they’re also packaged with straightforward instructions that walk you through every step of the process.
Additional resources
If you or someone you know is struggling with opioid addiction, there are many resources available to help. Here are a few:
- Visit 988 Suicide & Crisis Lifeline or dial 988
- SAMHSA National Helpline: 1.800.662.HELP (4357)
- FindTreatment.gov
- Minnesota Department of Health
- Welia Health Mental Health Services
By working together, we can help to prevent opioid overdose deaths in our community.
Know someone struggling with addiction? Educate yourself on Naloxone – it could be their ticket to a second chance. Step up and be the hero someone desperately needs right now!
Read more about how Welia Health is helping individuals addicted to opioids with Medication-Assisted Treatment in this blog post, Tackling addiction with more than one tool.
Disclaimer: The information provided in this blog post is for educational purposes only and should not be construed as medical advice. Please consult with a Welia Health healthcare provider if you have any questions about Naloxone or opioid overdose.









