Being safe
Medications
Please talk to your Welia Health provider about any medications or supplements you are taking if you are pregnant or thinking about becoming pregnant.
There may come a time during your pregnancy when you’re feeling under the weather and aren’t sure if you can take your regular over-the-counter (OTC) medication. Some medications are safe to take during pregnancy. But others are not, or their effects on your baby may not be known.
When you meet with your provider to confirm you are pregnant, ask what medications are acceptable to take and what medications you need to find alternatives for. Your provider will weigh the risks and benefits to help you know what’s safe.
Also, tell your provider about any alternative medicines or supplements you take, even if the label says “natural.”
Prenatal vitamins are safe and important to take when you’re pregnant. Ask your provider about the safety of taking other vitamins, herbal remedies and supplements. Most herbal preparations and supplements have not been proven to be safe during pregnancy.
If you get any new prescriptions while you’re pregnant, make sure the people who prescribe them know that you’re pregnant.
Generally, you should avoid taking any OTC medication while pregnant unless it is necessary.
To learn more, visit Treating for Two, a program developed by the Centers for Disease Control that aims to improve the health of women and babies by identifying the safest treatment options for common conditions before, during, and after pregnancy.
Smoking
Smoking may lead to serious health problems for your baby. If all smoking women would quit smoking during pregnancy, more than 5 percent of deaths among newborns could be prevented.
If you quit smoking, your baby will:
- Grow better because he or she will get more oxygen and food
- Have a better chance of being born full term and healthy
- Have a smaller chance of being miscarried or stillborn
- Have a smaller chance of dying of SIDS (sudden infant death syndrome)
If you quit smoking, you will:
- Have lowered chances of getting heart disease, cancer and lung problems
- Have improved blood flow, and the temperature of your hands and feet will return to normal
- Have a normal level of oxygen in your blood
- Be able to smell and taste food better
- Stop coughing
- Develop fewer wrinkles
- Save money
If you need help quitting tobacco, Welia Health offers a tobacco cessation program with one-on-one support from a Certified Tobacco Cessation Therapist. For more information or to schedule an appointment, call 320.225.3356. Services are available in Mora, Hinckley and Pine City. No referral is necessary.
Alcohol and drugs
There is NO safe amount of alcohol, marijuana or any street drug at any stage of pregnancy. Drinking any form of alcohol or using street drugs can harm a developing baby. The result can be stillbirth, miscarriage, low birth weight, birth defects, brain development issues and lifelong learning problems.
If you are concerned about any alcohol or street drugs you used before you knew you were pregnant, please talk with your provider. If you need help to stop drinking or using drugs, there are resources available.
If you are pregnant or are thinking about becoming pregnant, it is imperative that you don’t drink alcohol or use drugs. Alcohol and drugs pass through the placenta directly into your baby’s bloodstream. This can create lifelong problems for your baby, including physical and mental birth defects, heart defects, and problems in brain development and growth. Drinking alcohol increases your risk of miscarriage and preterm birth and can cause low birth weight.
Drinking alcohol while breastfeeding is also extremely unsafe; alcohol passes through breast milk directly to your baby.
If you are pregnant or breastfeeding and are having trouble not drinking alcohol, contact your provider about alcohol treatment programs or contact the National Council on Alcoholism and Drug Dependence at 1.800.622.2255 or www.ncadd.us.
Water
To make sure you stay adequately hydrated and to prevent constipation, hemorrhoids, and urinary tract or bladder infections, it’s important that you drink plenty of water while you’re pregnant. Aim for twelve (12) 8-ounce glasses of fluids each day, and try to choose water or low-fat milk whenever possible. You’ll need more fluid when you exercise, when the weather is hot, and if you’re ill with a fever. If your urine is colorless or light yellow, you know you’re drinking enough water.
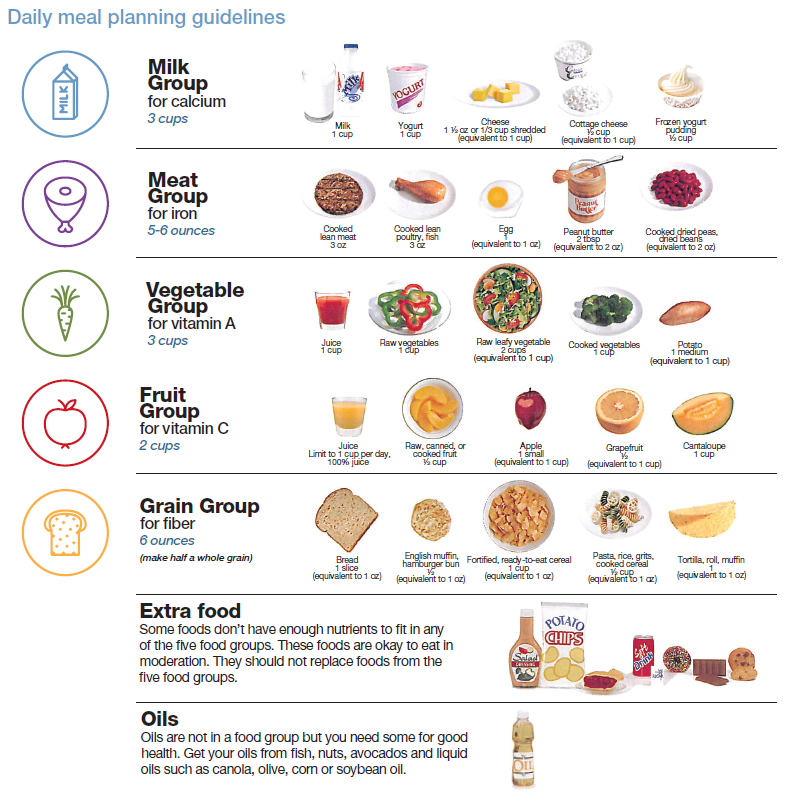
Weight gain
Generally, a weight gain during pregnancy of 25 to 35 pounds is recommended. Do not diet or skip meals, especially during late pregnancy, because the baby has a continuous need for calories. Your baby is growing 24 hours a day, so try to spread out your food intake. If excess weight gain is a problem, substitute quality for quantity. Avoid foods that contribute many calories but have little nutritional value.
Talk to your provider about any questions or concerns you may have related to healthy weight gain during pregnancy.
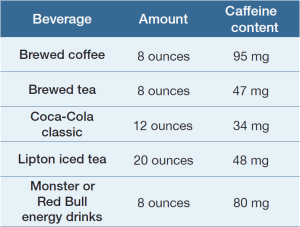
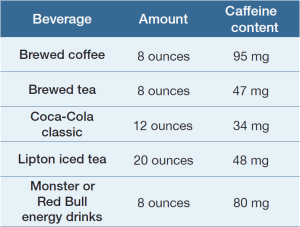
Caffeine
Some studies show a relationship between excessive caffeine intake and an increased risk of miscarriage, especially in the first trimester. Because of that, some providers recommend limiting caffeine to no more than 200 milligrams a day during early pregnancy. The caffeine content of some popular beverages is as follows:
Exercise
- Is it safe to exercise during pregnancy?
If you are healthy and your pregnancy is normal, it’s safe to continue or start most types of exercise during pregnancy. Swimming, stationary biking, brisk walking, gardening/yard work and modified yoga are often recommended. You may need to make a few changes, however, to ensure safety and comfort while exercising. Avoid activities that could result in falls, high impact to joints and abdominal strain—activities such as contact sports, heavy lifting, skiing, horseback riding, “hot yoga,” or pilates. If you are an experienced runner/jogger or racket-sports player, you should discuss these activities with your healthcare provider.
- What precautions should I take when exercising during pregnancy?
Drink plenty of water to prevent dehydration, avoid becoming overheated, wear a sports bra and consider an abdominal binder later in your pregnancy as needed for comfort. Always consult your healthcare provider before starting a new exercise routine, especially during pregnancy. If you are pregnant with multiples or have the following conditions or pregnancy complications, you should not perform aerobic exercise during pregnancy: placenta previa after 26 weeks of pregnancy, preeclampsia, severe anemia, certain lung and heart diseases, cervix insufficiency or cerclage.
- How much should I exercise during pregnancy?
The Centers for Disease Control and Prevention recommend that pregnant women get at least 150 minutes of moderate-intensity activity each week. This is best tolerated when split into intervals of 10-30 minutes. Moderate-intensity means you are moving enough to increase your heart rate and start sweating. You should still be able to talk normally but not sing. Monitor your heart rate; some experts recommend a sustained heart rate of no greater than 140 beats/minute during pregnancy. Stop exercising and call your healthcare provider if you have any of the following symptoms: vaginal bleeding, feeling dizzy or faint, shortness of breath before starting exercise, chest pain, headache, calf pain/swelling, sense of weakness, abdominal pain or contractions.
Adapted from the American College of Obstetrics and Gynecologists.
Saunas and hot tubs
Avoid sitting in saunas and hot tubs during the duration of your pregnancy. Both are very risky, as raising your core body temperature is hazardous to both you and your baby. There is a greater risk for dehydration, dizziness, lower blood pressure and birth defects, all symptoms associated with extreme heat situations.
HIV and AIDS
- Pregnancy and HIV
Infected women may pass HIV, or human immunodeficiency virus, to their children before or during birth or through breast milk. HIV is the virus that causes AIDS or acquired immunodeficiency syndrome. It is spread when body fluids (semen, vaginal secretions or blood) from an infected person enter the body of someone who is not infected. HIV is the third leading cause of death for women aged 25-44. If you are infected with HIV, there are ways you can protect your baby and your health.
- Protect yourself from HIV
- Do not have sex with multiple partners.
- Always use a latex condom and water-based lubricant during sexual intercourse.
- Always use a latex barrier when giving or receiving oral sex.
- If you have a new partner after becoming pregnant, ask to be re-tested.
- Do not share needles for piercing, applying tattoos or drug use.
- Talk with your partner(s) about AIDS, sex and drugs.
- Get tested for HIV
All pregnant women are routinely tested for HIV. Many women do not know they have been exposed to the virus because they don’t think they are at risk. The HIV test is a blood test that can be done during your prenatal visit. Tests are confidential, and results will go into your medical record.
- HIV test sites
If you do not want to be tested for HIV at your provider’s office, there are public Minnesota HIV counseling and testing sites.
- Hennepin County Red Door Clinic
525 Portland Ave S 4th Floor
Minneapolis MN 55415
612.348.6363
612.348.4729 TTY
- Ramsey County Department of Public Health, Clinic 555 (formerly Room 111)
555 Cedar St
St. Paul MN 55101
651.266.1255
No matter where you are tested, all positive HIV results are given to the Minnesota Department of Health. The report is private. If you test positive, a representative from the health department will contact you to discuss your treatment options.
For more information, call the Minnesota AIDS Line at 1.800.248.AIDS .
- If you are infected
If you have HIV, see your provider about getting the care you need to stay healthier longer. There is a 25 percent chance you will pass the virus to your baby, but medication is available to significantly reduce this risk.
Dental hygiene
It is important to keep regular dental check-ups during pregnancy, but remember:
- X-rays can be done, but with extreme caution.
- Hormonal changes during pregnancy can increase the risk of developing periodontal disease (gum disease).
- Brush and floss regularly to prevent or reduce oral health problems. The bacteria in your mouth are connected to preterm conditions.
Toxoplasmosis
Toxoplasmosis is an infection caused by a microscopic parasite called Toxoplasma Gondii, which is commonly found in cat feces. Although the infection generally results in a mild illness, it is risky during pregnancy because the parasite may infect the placenta and unborn baby. Throughout your pregnancy, it is important that you:
- Avoid changing cat litter.
- Wear gloves when gardening or when around sandboxes that may have been contaminated by cat feces.
- Avoid stray cats, especially kittens.
Group B Strep
Group B strep (streptococcus, GBS) is a bacteria that can be found in the vagina and/or rectum. Approximately 25% of healthy adult women carry this bacteria, which is not a sexually transmitted disease. It can, however, be transferred from a pregnant woman to her baby during childbirth. If GBS is passed to a baby during delivery, there is a risk to the baby of developing a life-threatening infection. About 35 to 37 weeks into your pregnancy, your provider will test for Group B strep using a vaginal and rectal swab. If the results are positive, showing you are a carrier, you will be treated with antibiotics during labor, as this can significantly reduce the risk of passing this bacteria to your baby.